Improving a vaccine with SARS-CoV-2 antigens

Dr. David Sancho’s team is studying whether the administration of immune response modulators can improve the effectiveness of various vaccines against the SARS-CoV-2 coronavirus
The response against the COVID-19 pandemic caused by the SARS-CoV-2 coronavirus infection is forcing science to sap its resources as quickly as possible to develop effective vaccines.
In Spain, Professor Mariano Esteban and Juan García Arriaza at the National Center for Biotechnology (CNB-CSIC) are leading the development of a vaccine prototype based on the same viral vector that managed to eradicate smallpox, which known as MVA. The design of this vaccine is based on the fact that this vector expresses the S protein of the virus, hoping that it will generate protective responses against it. From the CNIC, David Sancho’s group, in a collaboration led by Dr. Carlos del Fresno, has contributed to this development.
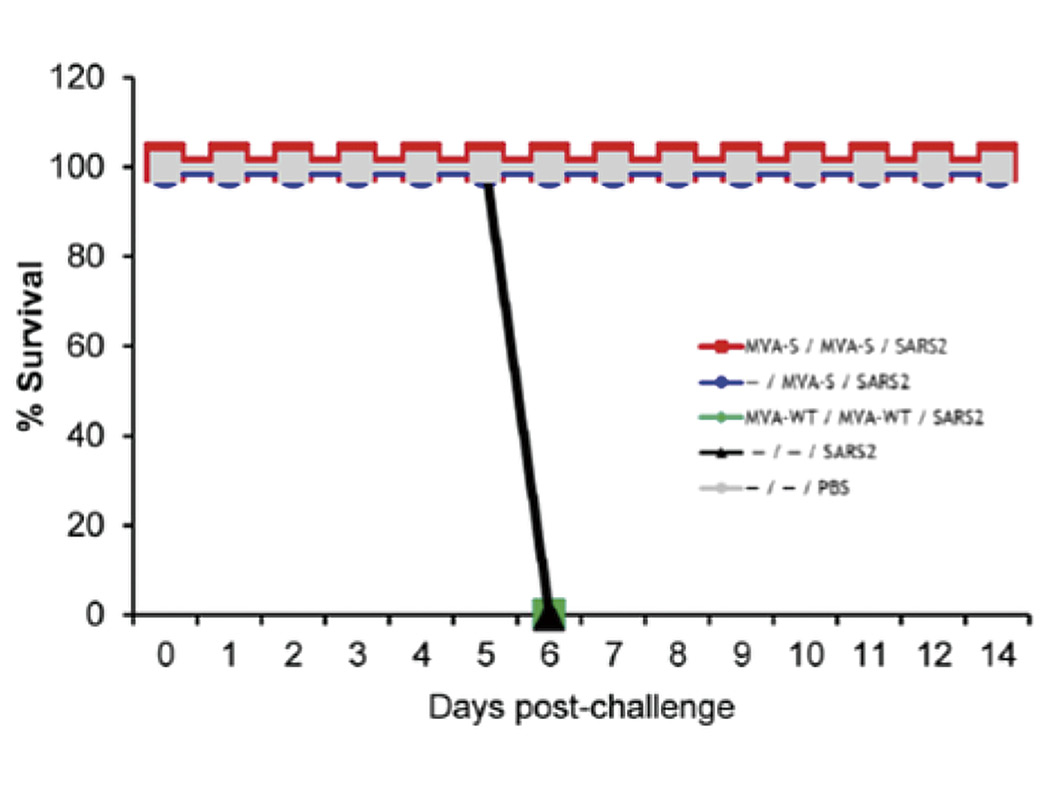
This vaccine has been tested in humanized mice that have the human version of the ACE2 receptor, a molecule that represents the entry point of the SARS-CoV-2 coronavirus into our cells. The results of this vaccine have been spectacular, with 100% efficacy in this mouse model, using different vaccination guidelines.
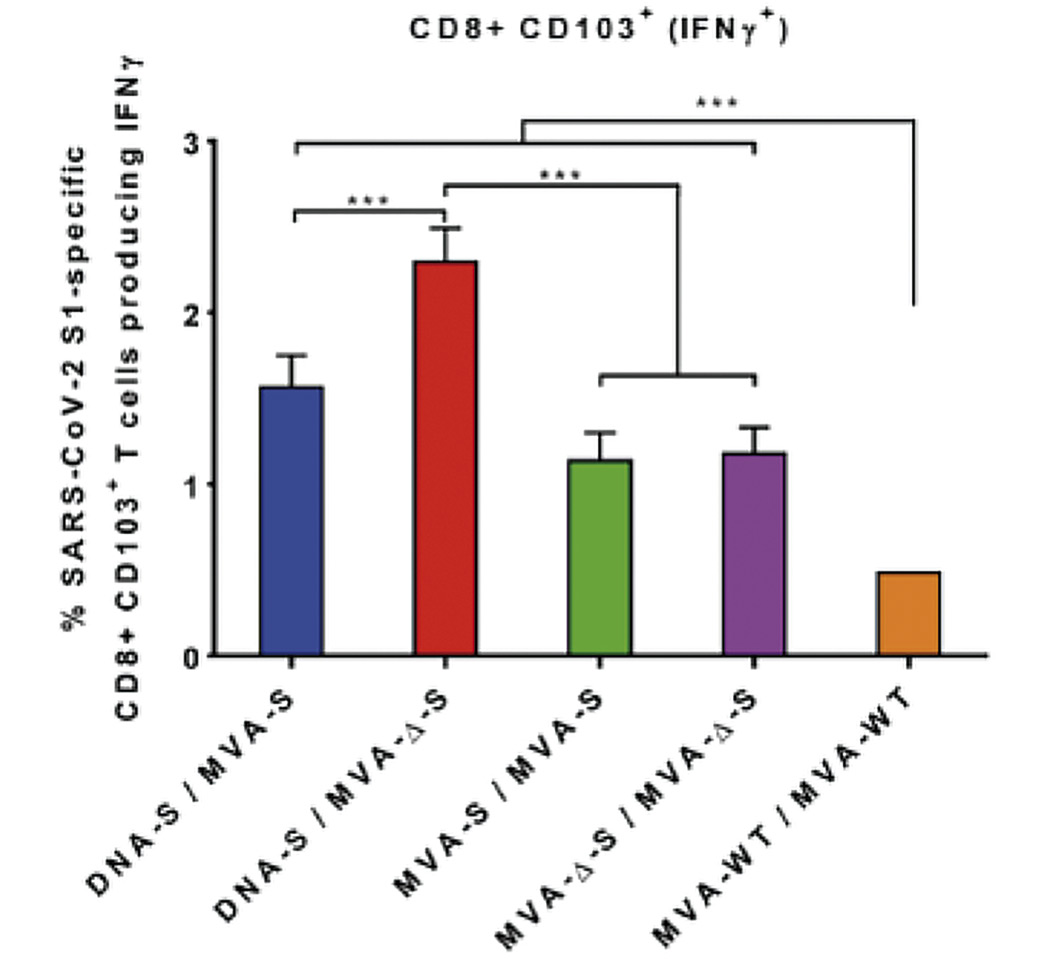
At the CNIC, a part of the study of the response generated by this vaccine has been carried out, analyzing the activation of certain immunological populations in which Dr. David Sancho’s laboratory has extensive experience in.
These experiments show that different variants of the vaccine manage to generate protective responses, as long as the vaccine contains the S protein of the coronavirus. The results of this research have been published in the prestigious magazine Journal of Virology.
Vaccines are intended to prepare the immune system against the virus that causes COVID-19. The protective effect of these vaccines is generated thanks to something called immunological memory. Until very few years ago it was believed that specific (adaptive) immunity was the only one that had memory (the ability to ‘remember’ previous pathogens - bacteria viruses ... - and trigger the response to defend the organism), while innate immunity (not specific for a particular pathogen) did not have it. Today it is known that innate immunity can be ‘trained’ to achieve a better response against subsequent unrelated infections, such as SARS-CoV-2, and that such training lasts for a long time.
In addition to this collaboration with the CNB-CSIC, Dr. David Sancho’s team is studying whether the administration of immune response modulators can improve the effectiveness of various vaccines against the SARS-CoV-2 coronavirus. This project, financed with €100,000 by Banco Santander through the “Together Solidarity Fund,” is making it possible to prove that it is possible to optimize the specific responses generated by vaccination.
CNIC researchers are testing the use of MV130 as an immune booster to enhance the ability of vaccines to generate an immune response against COVID-19. As Dr. Sancho explains, MV130 is a preparation that contains several inactivated bacteria that prevents morbidity and mortality in viral respiratory infections, such as influenza, which could boost and improve a vaccine with antigens of the SARS-CoV-2 virus.
In a project pending publication, it has been proven that MV130 protects against viral respiratory infections both by DNA viruses (Vaccinia -virus well known for its role already discussed as a vaccine in the eradication of smallpox disease) and by RNA viruses (Influenza/flu) in preclinical mouse models.
Similarly, “we have collaborated in a clinical trial that demonstrated effectiveness in protecting against recurring respiratory infections in children, which epidemiologically, are of viral etiology,” says Dr. Sancho. This clinical trial has been accepted for publication in the American Journal of Respiratory and Critical Care Medicine, the most prestigious international magazine of pulmonology and intensive care.
The researchers conclude that these results, would make it possible to improve the efficacy of vaccines, particularly in certain population segments or against variants of the pathogen that may reduce the effectiveness of the vaccine, contributing to better protection of the population against COVID-19.