JACC: Blood Thinners may Improve Survival among Hospitalized Covid-19 Patients
Research could change standard of care protocols to prevent clotting associated with coronavirus
Researchers from the Mount Sinai COVID Informatics Center found that treating hospitalized COVID-19 patients with anticoagulants (AC)— blood thinners that slow down clotting—may improve their chances of survival. The study, published in the The Journal of the American College of Cardiology, could provide new insight on how to treat and manage coronavirus patients once they are admitted to the hospital.
“This research demonstrates anticoagulants taken orally, subcutaneously or intravenously may play a major role in caring for COVID-patients, and these may prevent possible deadly events associated with coronavirus, including heart attack, stroke and pulmonary embolism,” says senior corresponding author Valentin Fuster, MD, PhD, Director of Centro Nacional de Investigaciones Cardiovasculares (CNIC) and Mount Sinai Heart, and Physician-in-Chief of The Mount Sinai Hospital. “Using anticoagulants should be considered when patients get admitted to the ER and have tested positive for COVID to possibly improve outcomes. However, each case should be evaluated an individualized basis to account for potential bleeding risk.”
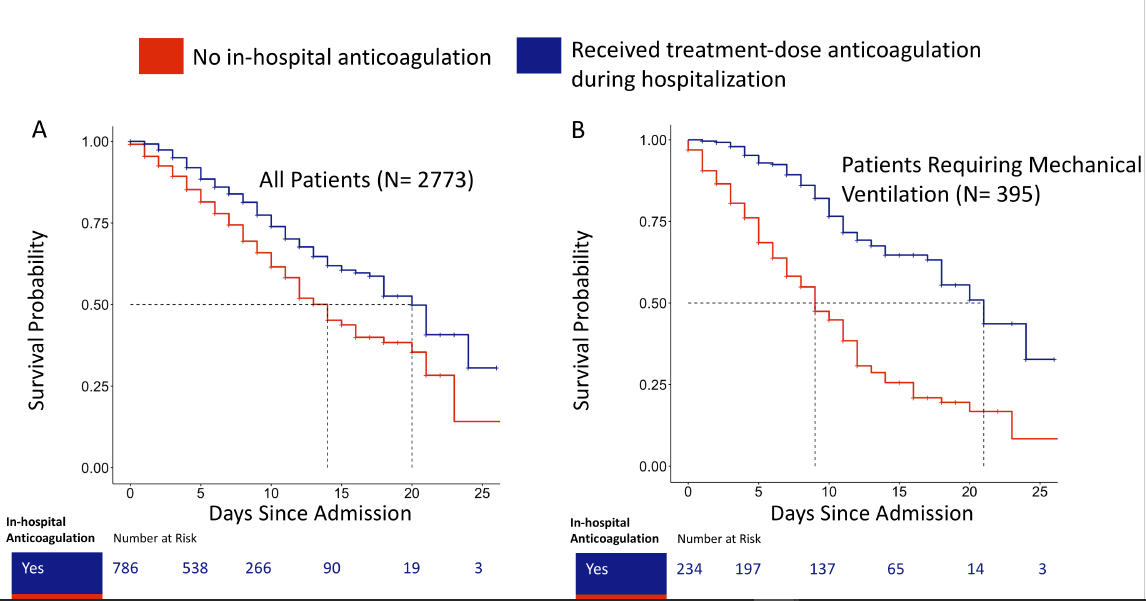
A team of investigators evaluated 2,773 confirmed COVID positive patients admitted to five hospitals in the Mount Sinai Health System in New York City between March 14, and April 11, 2020. They specifically looked at survival rates for patients placed on blood thinners versus those not placed on blood thinners. The researchers took certain risk factors into account before evaluating the effectiveness of anticoagulation, including age, ethnicity, pre-existing conditions, and those already on blood thinners.
Of the COVID-19 patients analyzed, 786 (28 percent) received a full-treatment dose of AC (a higher dose than what is typically given for blood clot prevention, usually given to those who already have clots or suspected to have clots). Treatment with AC was associated with improved hospital survival among COVID-19 patients both in and out of the intensive care unit setting. Of the patients who did not survive, those on AC died after spending an average of 21 days in the hospital, compared to the non-AC patients who died after an average of 14 days in the hospital. The effect of anticoagulation had a more pronounced effect on ventilated patients—62.7 percent of intubated patients who were not treated with AC died, compared to a 29.1 percent mortality rate for intubated patients treated with AC. Of the intubated patients who did not survive, those with no AC died after 9 days, compared to those on AC who died after 21 days.
All patients in the study had blood work taken when they arrived at the hospital, which included measuring various inflammatory markers. The study showed patients who received AC had higher inflammatory markers compared to patients not treated with AC. This may suggest patients with more severe illness may benefit from AC early on.
The observational study also explored the association of systemic AC treatment with bleeding events. Major bleeding was defined as 1) hemoglobin <7 g/dL and any red blood cell transfusion 2) at least 2 units of red blood cell transfusion within 48 hours or 3) a diagnosis code for major bleeding including intracranial hemorrhage, hematemesis, melena, peptic ulcer with hemorrhage, colon, rectal, or anal hemorrhage, hematuria, ocular hemorrhage, and acute hemorrhagic gastritis. Among those who did not receive AC, 38 (1.9%) patients had bleeding events, compared to 24 (3%) among those who received AC, p=0.2).
“As a cardiologist who has been on service caring for COVID patients for the last three weeks, I have observed an increased amount of blood clot cases among hospitalized patients, so it is critical to look at whether anticoagulants provide benefits for them,” says co-researcher Anu Lala, MD, Assistant Professor of Medicine (Cardiology) at the Icahn School of Medicine at Mount Sinai. “It’s important to note that further analysis and prospective studies are required going forward to determine the effectiveness for widespread use of AC in hospitalized COVID-19 patients.”
“Overall this study is opening the door for a more extensive study that will be carried out with 5000 COVID positive patients, where we will evaluate the effectiveness of three types of antithrombotic therapy –oral antithrombotic, subcutaneous heparin and intravenous heparin – and then perhaps engage our data for prospective clinical trials,” says senior author Girish Nadkarni, MD, Co-Director of the Mount Sinai COVID Informatics Center (MSCIC). “We are excited about these preliminary results that may have a positive impact on COVID patients and potentially give them a greater chance of survival, although more studies are needed.