Hepatology: Immune cells in the liver regulate body temperature
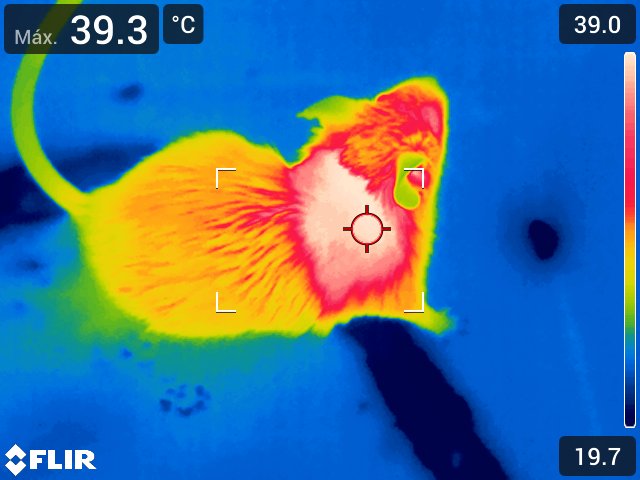
A study published in Hepatology demonstrates that the activation of thermogenesis in the livers of obese mice contributes to weight loss and improves diabetes symptoms
Scientists at the Centro Nacional de Investigaciones Cardiovasculares ( (CNIC) have discovered a complex network of connections between tissues that allows the liver to regulate body temperature. The research team found that the secretion of a molecule called interleukin 12 (IL-12) by immune cells present in the liver reduces heat generation by brown fat. The study is published in Hepatology.
When a person begins to gain weight, fat accumulates in adipose tissue. But eventually fat also accumulates in the liver, a process known as hepatic steatosis or fatty liver disease. This condition is associated with chronic inflammation mediated by inflammatory immune cells that secrete molecules responsible for the progression of the disease.
The new study reveals that one of these molecules, the protein IL-12, blocks the production of another protein, FGF21, in the liver. The decline in FGF21 results in reduced generation of heat by brown fat.
The Spanish scientists also discovered that the production of IL-12 by these immune cells is activated by the protein kinase p38, thus identifying a role for p38 in the regulation of liver endocrine function and whole-body metabolism. “We found that when we eliminated stress-kinase pathways in macrophages, these cells lost the capacity to adapt to a fatty diet and increased the production of IL-12, reducing the generation of heat,” explained María Crespo, first author on the study.
The inflammatory component of obesity is very important because it contributes to the development of diabetes, fatty liver disease, and liver cancer.
The study shows that IL-12 secreted by liver-infiltrating macrophages blocks the production of FGF21, a hormone produced in the liver that regulates body energy expenditure by promoting thermogenesis in brown fat. Although other groups have reported that thermogenesis is regulated by macrophages in fat tissue, this is the first study to demonstrate the regulation of thermogenesis by macrophages in another organ, and through a completely different mechanism.
When the researchers injected IL-12 into mice, they observed a rapid decline in the circulating levels of FGF21, detected within a few hours. “This connection between IL-12 and FGF21 has important implications for the treatment of the wasting disease associated with cancer, since treatment with IL-12 would in principle reduce bodily energy expenditure and could limit weight loss in cancer patients,” noted co-author Dr. Magdalena Leiva.
The article also describes the link between IL-12 and the prognosis of patients with fatty liver disease. As study leader Dr. Guadalupe Sabio explained, “we found that IL-12 is elevated in the livers of obese patients, and this is directly associated with worse liver damage. This result indicates that IL-12 contributes to the progression of steatosis and could be used as a new disease marker and as a target for the treatment of this disease.”
The study highlights the importance of thermogenesis in the control of obesity, since activation of this process burns energy, promoting weight loss and ameliorating diabetes. As the authors point out, there are already drugs on the market that reduce the levels of IL-12, and these could in principle be used to treat patients with obesity or metabolic syndrome.
In addition to the CNIC group led by Dr. Sabio, the study also included contributions from scientists in the Spanish research network on the pathophysiology of obesity and nutrition (CIBERobn), the Universidad Rey Juan Carlos, and Hospital Universitario de Salamanca.
The study received funding from the following grant awarding bodies: Asociación Española contra el Cáncer, EFSD, Lilly European Diabetes Research Programme; Ministerio de Ciencia, Innovación y Universidades; Comunidad de Madrid; Fundación BBVA; Unión Europea 7th Framework Programme.