Cell Genomics: CNIC scientists reveal how the cellular energy system evolved—and how this knowledge could improve the diagnosis of rare genetic diseases
CNIC researchers have uncovered the evolutionary logic of the OxPhos system—the cell’s “engine”—and developed a tool to detect mutations that cause mitochondrial disease
Mitochondria are the body’s “energy factories,” and their proper function is essential for life. Inside mitochondria, a set of complexes called the oxidative phosphorylation (OxPhos) system acts like a biochemical assembly line, transforming oxygen and nutrients into usable energy.
Now, the study, led by the GENOXPHOS group at the Spanish National Centre for Cardiovascular Research (CNIC) and the Biomedical Research Networking Centre in the area of Frailty and Healthy Ageing (CIBERFES), and directed by Dr. José Antonio Enríquez, has revealed how this system evolved over millions of years—from the first vertebrates to modern humans. “Understanding this evolution helps explain why some genetic mutations cause rare but serious diseases that affect the OxPhos system,” say José Luis Cabrera lead author of the article, whose research is supported by the ‘la Caixa’ Foundation.
Published in Cell Genomics, the study describes the molecular evolutionary strategies of the OxPhos system, the main site of metabolic and energy integration in the cell. It also shows how this information can be used to identify mutations that cause disease.
Working in collaboration with Fátima Sánchez-Cabo, head of the CNIC Computational Systems Biomedicine group, the researchers analyzed the interaction between the two types of DNA that encode OxPhos proteins: nuclear DNA (inherited from both parents) and mitochondrial DNA (inherited only from the mother).
The OxPhos system, explains José Antonio Enríquez—head of the CNIC Functional Genetics of the Oxidative Phosphorylation System (GENOXPHOS) group—comprises five large protein complexes: four that transport electrons and one, called ATP synthase, that produces ATP, the cell’s molecular “fuel.”
“These complexes can work individually or in combination, depending on the cell’s energy needs. Together, they are made up of 103 proteins encoded by two different genomes: nuclear and mitochondrial,” Enríquez explains. “While nuclear DNA changes slowly over time and gains variation through genetic mixing during reproduction, mitochondrial DNA evolves much more rapidly but is passed only through the maternal line.”
Dr. Cabrera adds that the proteins encoded by mitochondrial DNA form the core of the respiratory complexes, “so proper function depends on precise compatibility between the nuclear and mitochondrial components.”
The study also introduces an innovative new tool: ConScore, a predictive index that assesses the clinical relevance of mutations in the 103 OxPhos proteins. “ConScore is based on the evolutionary divergence of these proteins across vertebrates—including primates and other mammals—and complements human population genetic data,” says Enríquez.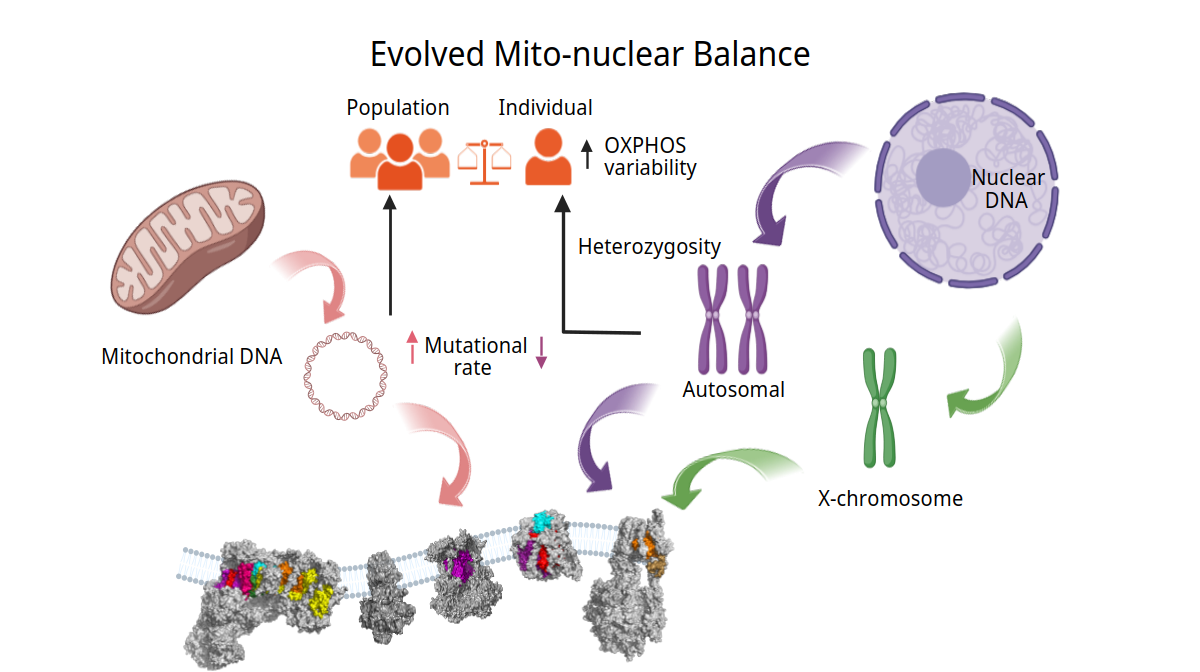
The authors affirm that ConScore provides a new framework for interpreting potentially pathogenic mutations, opening the door to improved diagnosis and treatment of mitochondrial diseases.
Ultimately, the researchers conclude, this study not only advances our understanding of how human cells evolved, but also brings us closer to new solutions for patients with rare genetic disease.
The study has received funding from the European Union's NextGenerationEU/Recovery, Transformation and Resilience Plan/PRTR, CIBERFES; Fundación ‘la Caixa’,Human Frontier Science Fundation; Severo Ochoa grant awarded by MICIU/AEI and the European Social Fund (ESF invests in your future).











